A New Chapter of Menopause
Menopause changes everything. One day, your favorite jeans fit perfectly; the next, you’re battling stubborn belly fat, unpredictable hot flashes, and energy crashes that make 3 PM feel like midnight. If you’ve tried every diet without lasting results, intermittent fasting post menopause might be the missing piece. However, IF is not suitable for all unless you follow your plans and steps with full effort and consistency.

Unlike premenopausal women, postmenopausal bodies face unique challenges: plummeting estrogen levels, slower metabolic rate, and increased insulin resistance. These shifts make weight loss harder and raise risks for heart disease, bone loss, and mood swings. The good news? Emerging research shows that strategic intermittent fasting can reboot metabolism, improve insulin sensitivity, and even ease menopausal symptoms, if done right.
Intermittent fasting post menopause
Intermittent fasting post menopause isn’t about skipping meals or starving yourself, it’s about working with your body’s new rhythm instead of fighting against it. Think of it as a reset button, helping your metabolism catch up with the changes that menopause brings. By narrowing your eating window and giving your body time to rest and repair, many women over 50 are finding more energy, less belly fat, and a better handle on blood sugar swings. It’s not a magic fix, but when done right, it can feel pretty close.
The Menopause-Metabolism Connection: Why Your Body Resists Weight Loss
You’re not imagining it; the menopausal weight gain is different. It’s not just a matter of eating too much or moving too little. It’s a shift in your body’s biology, a recalibration of everything from hormones to how your cells use energy. And for many postmenopausal women, it feels like the body that once responded to healthy eating and regular exercise is now stubbornly doing its own thing.
Let’s break down exactly what’s happening behind the scenes.
1. Estrogen’s Quiet Exit, and Its Big Impact on Fat Storage
Before menopause, estrogen plays a quiet but powerful role in shaping our metabolism. It helps distribute fat more evenly across the body (often in the hips and thighs), regulates hunger hormones like ghrelin and leptin, and keeps insulin levels balanced. But after menopause, when estrogen levels drop, all of those changes.
Suddenly, the body starts storing more fat around the abdomen, also known as visceral fat, a type that surrounds internal organs and is linked to a higher risk of heart disease and metabolic syndrome.

You might notice that cravings, especially for sugar or carbs, hit harder. That’s because with less estrogen, your cells become less sensitive to insulin, making blood sugar levels spike and crash more easily. Lower estrogen levels lead to higher fat mass, especially around the abdomen.
The result? More fat storage, more mood swings, and Slower fat burning. Your body clings to stored fat more stubbornly, even on a low-calorie diet.
2. The Silent Thief – Muscle Loss and a Slowing Metabolism
Muscle isn’t just for strength; it’s a metabolic powerhouse. The leaner muscle mass you have, the more calories your body burns, even at rest. But starting as early as your 40s, women begin to lose 3–5% of muscle mass per decade. After menopause, this decline picks up speed.
This matters because less muscle means a slower metabolic rate. So even if your calorie intake stays the same, your body may start gaining fat. And without enough physical activity, the shift toward muscle loss and fat gain only gets worse.
That’s why so many postmenopausal women say, “I haven’t changed anything, but I’m gaining weight.” The rules have changed, and your body didn’t send a memo.
3. Insulin Resistance and the Blood Sugar Roller Coaster
One of the most overlooked symptoms after menopause is blood sugar instability. Even women who never struggled with glucose issues before may find themselves dealing with energy crashes, cravings, and even early signs of insulin resistance.
When cells don’t respond well to insulin, glucose stays in the bloodstream instead of being used for energy. This leads to:
Higher fasting glucose levels
More fat is stored around the belly.
Tiredness and brain fog, especially after meals
This isn’t just a weight issue, it’s a long-term health concern. Insulin resistance increases the risk of type 2 diabetes, cardiovascular disease, and cognitive decline if left unaddressed.
4. Bone Health: The Hidden Cost of Hormonal Change
Estrogen isn’t only about reproduction; it’s also one of your bones’ best friends. It helps maintain bone density, and once levels plummet, bone loss accelerates, increasing the risk of osteoporosis.

This is especially important when considering dietary changes like intermittent fasting post menopause. If you’re fasting without prioritizing nutrients, especially calcium, vitamin D, and protein, you may unintentionally compromise your bone health.
A Shift That Feels Personal
These changes don’t just happen on charts or in lab reports. They show up in the way you feel in your body, how your clothes fit, how your brain functions, how you relate to food, and how confident you feel in your skin. And when traditional advice like “eat less, move more” doesn’t seem to work anymore, it’s easy to feel defeated.
But here’s the truth: Your body isn’t broken. It’s just changing. And it needs a different kind of support. Finding the accurate way for your weight loss journey with intermittent fasting.
This is where intermittent fasting post menopause enters the conversation, not as a trend, but as a strategy aligned with how your body now functions. When approached mindfully, it can help reverse some of these metabolic shifts and restore a sense of balance, strength, and energy.
The Benefits of Intermittent Fasting After Menopause
Intermittent fasting isn’t about eating less, it’s about changing when you eat and allowing your body time to reset. For older women, especially in midlife or postmenopause, this can be a game-changer.
1. Supports Weight Loss & Fat Burning
During periods of fasting, the body shifts from burning glucose to burning fat. This is what many call “fat-burning mode.” It leads to weight loss, especially when paired with a focus on nutrient-dense, whole foods.
A new study (2025) (JOMH) found that post-menopausal women practicing time-restricted eating (like a 14:10 fasting window) saw a significant decrease in body weight, who lost 3x more belly fat while preserving muscle mass than those just cutting calories. Why?
- Longer periods of fasting force the body to tap into fat stores.
- Lower insulin levels = less fat storage.
Key Insight: Pair IF with protein-rich meals to protect muscle mass.
2. Enhances Insulin Sensitivity
One of the most powerful health benefits of IF is its ability to reduce insulin resistance. By giving the body a break from constant food intake, blood sugar stabilizes, and insulin sensitivity improves.
Studies show that time-restricted eating, especially an 8-hour window, helps regulate glucose levels and may lower the risk of type 2 diabetes in postmenopausal women.
Another study from Aviva Romm’s clinic shows that fasting for 12+ hours improves insulin sensitivity, critical for midlife women. One patient group saw a 20% lower fasting glucose in 8 weeks!
3. Improves Heart Health
As LDL cholesterol, high blood pressure, and inflammation often rise after menopause, heart disease risk also climbs. IF has shown beneficial effects on these markers, contributing to better cardiovascular health.

4. Eases Menopausal Symptoms
Regular fasting can lower oxidative stress, ease joint pain, and support brain function. Many women report fewer hot flashes, better sleep, and more stable energy levels. While IF won’t increase estrogen levels, it helps balance hunger hormones like leptin and ghrelin, reducing cravings and irritability.
5. Mental Clarity & Mood Support
Say goodbye to brain fog. Fasting gives your gut and brain a break. It supports the gut microbiome, which has direct links to mental health. Women also notice more emotional balance, fewer mood swings, and greater focus. Autophagy (cellular cleanup during fasting) may reduce brain fog.
Best Fasting Methods for Postmenopausal Women (Ranked by Safety & Efficacy)
Not all fasting approaches are created equal, especially for postmenopausal women dealing with unique metabolic and hormonal shifts. The key is to choose a method that supports insulin sensitivity, protects muscle mass, and works with your body’s circadian rhythm, not against it. Below are the top intermittent fasting methods, carefully ranked by safety and effectiveness for postmenopausal women.
1. Gentle Time-Restricted Eating (12–14 Hour Fast)
Best for: Hormonal balance, sustainable weight management, and beginners
How it works:
Stop eating after dinner (around 7 PM), then have your next meal between 7–9 AM. This creates a natural 12–14 hour fasting window without harsh restrictions or hunger pains.
Why it’s ideal for older women:
This gentle method aligns beautifully with your natural circadian rhythm, allowing your metabolism and digestive system to reset overnight. It lowers insulin levels while keeping cortisol (the stress hormone) in check, especially important for post-menopausal women who may already be prone to hormonal imbalances.
Additional benefits:
- Reduces nighttime insulin spikes
- Supports healthy blood sugar levels
- Promotes better sleep and energy levels
- Eases hot flashes and improves mood swings
Human Tip: You won’t even feel like you’re fasting. Most of the time, you’re just sleeping!
2. The Modified 5:2 Method (Best for Weight Loss & Flexibility)
Best for: Fat loss, insulin resistance, and flexible lifestyles
How it works:
Eat normally for five days a week (within a normal calorie intake), and on two non-consecutive fasting days, reduce your intake to about 600–800 calories. Focus on high-protein foods, healthy fats, and plenty of fiber to stay full and support muscle mass.

Science speaks:
According to a new study by Cienfuegos S (2023), women who followed a modified 5:2 diet for 12 weeks experienced a 6% reduction in body fat, without compromising bone health or mental clarity.
Why it’s effective:
This method works well for postmenopausal women because it creates a calorie deficit without constant deprivation. It improves insulin sensitivity, reduces body fat, and helps reset your appetite, thanks to lower hunger hormone activity.
Pro tip: Schedule your fasting days on lighter, less active days to avoid fatigue. Think Sunday and Wednesday.
3. Overnight Fasting (13-Hour Fast)
Best for: Breast health, blood sugar control, and ease of practice
How it works:
Fast for about 13 hours overnight, such as finishing dinner by 8 PM and eating breakfast at 9 AM.
Backed by research:
A large study published in JAMA (2020) found that post-menopausal women who fasted for at least 13 hours overnight had a 20% lower risk of breast cancer. That’s a huge win for long-term health benefits without extreme effort.
Why it’s beginner-friendly:
This low-stress fasting style fits easily into your daily routine and doesn’t disrupt your social or family meals. It’s an ideal first step if you’re new to fasting but still want to experience the positive effects.
Added perks:
Encourages healthy weight maintenance
Supports gut microbiome healing
Minimizes blood sugar spikes and oxidative stress
Fasting Methods to Avoid (Unless Closely Supervised)
While fasting can have beneficial effects, not every method is suitable, especially when bone loss, hormonal changes, and energy levels are already in flux. Always approach a healthcare professional to get the right methods and steps to follow. These methods should be approached with caution:
Warrior Diet (20:4 Method)
Fasting window: 20 hours
Eating window: 4-hour evening feast
This intense plan includes eating small amounts of healthy fats or amino acids during the day, followed by a large meal at night.
Why it’s risky for postmenopausal women:
Can cause adrenal stress and extreme fatigue
Increases the risk of nutrient deficiencies if not monitored closely
May exacerbate hot flashes, joint pain, or mood swings due to a lack of fuel during the day
Verdict: Not recommended unless under supervision by a registered dietitian or healthcare provider.
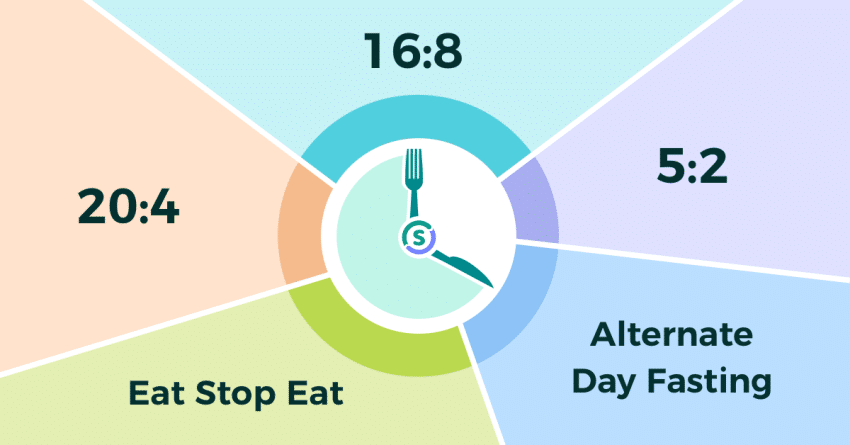
Alternate-Day Fasting
How it works: Eat normally one day, restrict to ~500 calories the next.
Concerns for older women:
May worsen bone loss and lead to muscle breakdown
Can interfere with hormone levels and lead to sleep disturbances or brain fog
Not suitable for those with heart disease or other medical conditions without close monitoring
Remember: Too extreme for most postmenopausal women. Reserve only for experienced fasters with medical guidance.
You can also read: Best Intermittent Fasting for Women Over 50
Final Thoughts on Choosing the Right Method
When choosing the best intermittent fasting post menopause plan, always consider your current health issues, daily routine, and personal goals. The most effective plan is the one you can follow with joy, not dread. Whether it’s a gentle overnight fast or a flexible 5:2 routine, consistency matters far more than intensity.
And remember:
✔️ Prioritize nutrient-dense foods rich in calcium, protein, and healthy fats
✔️ Stay hydrated with herbal teas or black coffee during fasting hours
✔️ Pair your fasting plan with physical activity, especially strength training, to protect your bone health and preserve muscle mass
Potential Risks & How to Avoid Them
1. Bone Loss: Protect Your Foundation
After menopause, estrogen levels drop, and that can accelerate bone thinning. Fasting without proper nutrition may make this worse, especially if you’re skipping meals that would normally include calcium-rich foods.
What to do:
Aim for at least 1,200 mg of calcium daily from sources like leafy greens, dairy, almonds, or fortified plant milks. Also, try to walk, climb stairs, or do light strength training; these activities signal your bones to stay strong.
Pro Tip: Pair calcium with vitamin D (through sun exposure or supplements) to help with absorption.
2. Muscle Loss: Don’t Lose Strength Along the Way
One of the sneakiest effects of menopause is the slow but steady loss of muscle mass. Fasting without enough protein or movement can speed this up, leading to weakness and slower metabolism.
What to do:
Make protein the star of every meal, think eggs, lentils, fish, tofu, Greek yogurt, aiming for around 30 grams per meal. Combine this with resistance workouts like bodyweight exercises or light weights at least twice a week.
Why it matters: Muscle isn’t just for strength; it helps regulate blood sugar, burn calories, and support balance and mobility as you age.
3. Hormonal Imbalance: Don’t Overdo It
Too much or too aggressive fasting can put stress on your adrenal glands, which are already working overtime during menopause. This can lead to worsened hot flashes, dizziness, fatigue, and even increased anxiety.

What to do:
Start with a gentle 12-hour overnight fast (like 7 PM to 7 AM), and listen to your body. If you notice signs of burnout or mood swings, it might be time to scale back or adjust your approach.
Bonus Tip: Avoid caffeine on fasting days, as it can spike cortisol (your stress hormone) and make symptoms worse.
Nutrient Deficiencies
As you begin intermittent fasting post menopause, it’s essential to pay attention to your nutritional intake, especially because hormonal changes can affect how your body absorbs and uses certain nutrients. You can also rely on the Galveston diet to obtain better results.
Key nutrients to focus on:
Magnesium – Found in nuts, seeds, leafy greens, and yes, dark chocolate. Magnesium helps with sleep quality, muscle relaxation, and may even ease mood swings and anxiety.
Vitamin D – Crucial for bone strength and immune function. Many postmenopausal women are deficient in vitamin D, especially if sun exposure is limited. Consider foods like salmon, fortified dairy, or supplements if advised by your doctor.
Omega-3 Fatty Acids – These healthy fats support brain health, reduce inflammation, and may ease joint stiffness. Include fatty fish (like salmon or mackerel), chia seeds, and walnuts regularly.
Pro Tip: Partner with a registered dietitian who specializes in women’s health and menopause. They can help create a fasting-friendly meal plan that keeps you well-nourished, energized, and on track with your goals, without the guesswork.
Note: In the following days after starting IF you might encounter negative side effects, which can usually be surpassed, especially if you stay hydrated with water, herbal teas, or black coffee
What About Perimenopausal or Pre-menopausal Women?
IF can work for pre-menopausal women, too, but it’s more delicate. Women still experiencing a menstrual cycle need to pay attention to hunger cues, hormonal changes, and menstrual flow. Some prefer gentler fasting, especially during the luteal phase.
The Best IF guide for women on Amazon
Ready to feel like you again? This powerful guide is crafted for women who are done with fads and ready for real, lasting change. Backed by science and written with heart, it shows you how to balance hormones, fire up your metabolism, and lose weight without punishing diets or counting every bite. It’s time to take back control of your body and your confidence, on your terms
1. Can intermittent fasting help with a low sex drive or sexual dysfunction?
Yes, it can. Intermittent fasting helps improve blood circulation, balances hormones, and even lifts your mood, all of which play a role in sexual well-being. Many women find that their libido improves as their body adjusts to fasting.
2. Will fasting make my hot flashes worse?
At first, it might feel like your hot flashes are getting worse. That’s just your body adjusting. The good news? Most women notice a big improvement after about 4–6 weeks. Just make sure you’re staying hydrated, and adding electrolytes can help too.
3. Can I still drink coffee while fasting?
Absolutely! Black coffee (without sugar or milk) is totally fine during your fasting window. It can help reduce appetite and support fat burning.
4. What if I have diabetes or thyroid issues? Is fasting safe?
It can be, but you’ll want to check in with your doctor first. Intermittent fasting may help balance blood sugar, but you might need to adjust your medications or monitor certain symptoms more closely.
5. I’m not menopausal yet, could fasting mess up my cycle?
It’s possible, especially if the fasting window is too long or you’re not eating enough during eating hours. If you’re still having periods, start slowly with a gentle fasting routine (like 12:12 or 14:10) and see how your body responds.
6. Is intermittent fasting safe if I have a medical condition?
In many cases, yes, but it depends on the condition. For people with diabetes, heart disease, or other chronic illnesses, it’s important to talk to your healthcare provider before starting. They can help you do it safely.
7. How soon will I see changes in my body?
Most women notice better energy in just 1–2 weeks. For weight loss or visible changes, give it at least 4–6 weeks. Remember, slow progress is still progress, consistency matters more than speed.
Conclusion – Listening to Your Body, One Fast at a Time
Intermittent fasting after menopause isn’t about strict rules or chasing numbers. It’s about reconnecting with your body, one that’s wise, resilient, and still changing. It’s about finding a rhythm that suits your new chapter, not punishing yourself for what no longer works. Finding a daily routine that nourishes your body, calms your mind, and aligns with the new pace of life after menopause. When done mindfully, intermittent fasting can bring balance, clarity, and strength. It doesn’t just help with weight management; it helps you feel at home in your body again.
So, whether you’re exploring fasting to shed body weight, improve insulin sensitivity, or ease menopausal symptoms.
And remember, this isn’t just about food or hours on a clock. It’s about healing, balance, and coming home to your body, gently and on your terms.
Start gently, with a 12-hour fast.
Listen to your body, always.
Focus on nourishing foods, not just fasting windows.
Move your body regularly. Walk. Lift. Dance.
And most of all, be kind to yourself.
Have you tried intermittent fasting post menopause? Share your experience below, your story might just be the inspiration another woman needs.



