Introduction
Intermittent fasting has taken the health and wellness world by storm, with millions of people embracing this lifestyle for its numerous health benefits, from weight loss to improved insulin sensitivity. But as with any lifestyle change, questions arise, especially when it comes to managing health conditions or taking medications during the fasting period. One of the most common questions is: Does Tylenol break intermittent fasting?
If you’ve ever found yourself Googling this question or scrolling through TikTok for answers, you’re not alone. Pain relief is a necessity for many, but the fear of breaking a fast can leave you wondering whether to pop that pill or tough it out. In this comprehensive guide, we’ll dive deep into the science, myths, and practical advice surrounding Tylenol and intermittent fasting. By the end, you’ll have all the information you need to make an informed decision, without compromising your fasting goals.
What Is Intermittent Fasting, and Why Does It Matter?
Intermittent fasting (IF) is a popular eating pattern that alternates between periods of fasting, where no food is consumed, and designated times for eating. It’s not just a diet but lifestyle changes have gained popularity for their ability to improve health markers like insulin sensitivity and weight loss This approach stands in contrast to conventional diets, which typically emphasize the types of foods you should eat. Instead, IF shifts the focus to when you consume your meals. Among the various techniques,
The 16:8 method is one of the most common, where individuals fast for 16 hours and allow an 8-hour window for eating.
Other methods of intermittent fasting include alternate-day fasting, where individuals alternate between days of regular eating and fasting,
and the 5:2 diet, which involves eating normally for five days and significantly reducing calorie intake on two non-consecutive days.

The benefits of intermittent fasting are well-supported by research, highlighting a range of positive health outcomes. These include improved insulin sensitivity, which can lead to better blood sugar control, and significant weight loss due to reduced calorie intake over time.
Also, several studies suggest that IF may enhance brain function by promoting neuroplasticity and reducing oxidative stress. Intermittent fasting is associated with a lowered risk of chronic diseases, such as heart disease and diabetes, making it a compelling strategy for those looking to optimize their health and longevity. To fully experience these remarkable benefits, it is essential to maintain a genuine fasting state during fasting periods, which means strictly avoiding any caloric intake.
The Role of Medications in Intermittent Fasting
Many people rely on prescription, OTC, or supplements to manage health conditions. Whether it’s a type of medication like Tylenol or a class of medications such as non-steroidal anti-inflammatory drugs (NSAIDs), understanding how they interact with fasting is crucial. The question is: Do these medications break your fast?
This is especially relevant for pain relievers like Tylenol (acetaminophen), which millions of people use for headaches, menstrual cramps, or chronic pain. Some medications, particularly those containing calories or requiring food for absorption, can disrupt a fasting state.

Fat-Soluble Vitamins (A, D, E, K): These require dietary fat for proper absorption, meaning they are usually taken with food. If a supplement or medication contains added oils or fat for absorption, it could break a fast by triggering digestion and metabolic responses. However, Tylenol does not require fat for absorption, making it safe to take while fasting.
Water-soluble Vitamins (C, B-complex): These dissolve in water and are absorbed easily without food. Since Tylenol is also water-soluble, like these vitamins, it does not need food or fat for absorption. This similarity further supports the idea that taking Tylenol during fasting does not interfere with the fast.
Does Tylenol Break Intermittent Fasting?
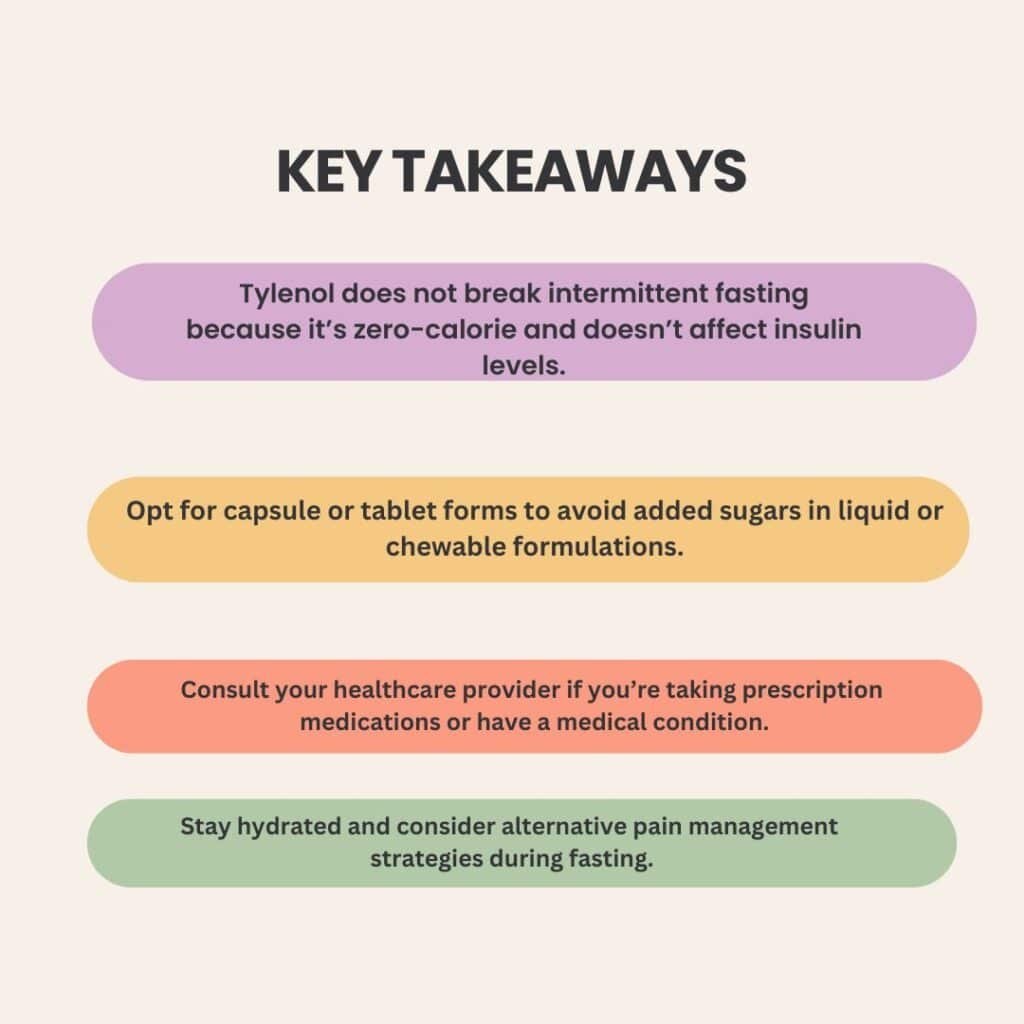
The short answer is No, taking Tylenol (acetaminophen) in pill or caplet form won’t break your fast. It has zero calories and doesn’t spike insulin, meaning it doesn’t contain any calorie content or macronutrients (carbs, fats, or proteins) that could trigger an insulin response or disrupt your fasting state. So it won’t interfere with the benefits of intermittent fasting. That said, be mindful of liquid or chewable versions, as they often contain sweeteners or a tiny amount of sugar, which could have a slight impact, especially if you’re following a super strict fasting state. If you’re unsure, always check the original bottle or chat with your doctor.
How Tylenol Works in the Body
The Science Behind Tylenol
Tylenol, or acetaminophen, is a widely used pain reliever and fever reducer. Unlike such drugs as NSAIDs, which can cause stomach problems or kidney damage with prolonged use, Tylenol is gentler on the digestive system. Unlike nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen, Tylenol doesn’t have anti-inflammatory properties. Instead, it works by blocking pain signals in the brain and reducing fever.

One of the key advantages of Tylenol is that it’s gentle on the stomach lining, making it a preferred choice for individuals with stomach ulcers or digestive issues. However, it’s metabolized by the liver, and taking large doses can lead to liver damage. This is why it’s crucial to stick to the recommended dosage.
Forms of Tylenol – Capsules, Tablets, and More
Tylenol comes in various forms, including capsules, chewable tablets, and liquid suspensions. While most forms are calorie-free, some liquid formulations or chewable tablets may contain small amounts of sugar or other additives. If you’re fasting, opt for the capsule or tablet form to avoid any unnecessary calories.
Tylenol and Intermittent Fasting – What You Need to Know
Caloric Content and Insulin Response
The primary concern with taking any medication during fasting is whether it contains calories or triggers an insulin response. For example, some vitamin supplements or fasting diets may include small amounts of calories, but Tylenol’s number of calories is zero, making it fasting-friendly. As mentioned earlier, Tylenol is zero-calorie and doesn’t contain macronutrients, it won’t spike your blood sugar levels or interfere with fat burning.

However, if you’re taking Tylenol with a small amount of food (to prevent stomach upset), this could technically break your fast. The same applies to liquid formulations with added sugars. To stay fast, take Tylenol with water on an empty stomach.
Impact on Fasting Benefits
One of the main goals of intermittent fasting is to improve insulin sensitivity and promote fat burning. Since Tylenol doesn’t affect blood sugar levels or insulin response, it won’t negate these benefits. However, if you’re fasting for autophagy (cellular repair) or gut health, it’s worth noting that any substance, including medications, could theoretically have a minor impact. That said, the effect is likely negligible.
Common Misconceptions About Tylenol and Fasting
Myth 1 – All Medications Break a Fast
Not all medications are created equal. For instance, vitamin D supplements or amino acids like non-essential amino acids may have a calorie content that could break your fast, but Tylenol does not. While some medications contain calories or require food for absorption, others, like Tylenol, are calorie-free and safe to take during fasting. Always check the label or consult your healthcare provider if you’re unsure.
Myth 2 – Tylenol Causes Stomach Upset on an Empty Stomach
Unlike NSAIDs, which can irritate the stomach lining and increase acid production, Tylenol (acetaminophen) is much gentler on the digestive system. Most people can take it without issues, but those with sensitive stomachs may still experience mild discomfort. If needed, a small sip of water can help, though consuming food alongside it may break your fast.
Myth 3 – Fasting Makes Tylenol Less Effective
Fasting does not interfere with Tylenol’s ability to relieve pain or reduce fever. Since it is absorbed primarily in the small intestine and does not rely on food for activation, its efficacy remains unchanged. An empty stomach may even promote quicker absorption, ensuring faster relief without compromising its overall effectiveness.
When to Take Tylenol During Intermittent Fasting
Best Time to Take Tylenol
If you’re following a 16:8 fasting schedule, the best time to take Tylenol is during your fasting window. However, if you experience the following symptoms like nausea or dizziness, consult your health care provider to adjust your medication regimen, especially if you’re dealing with pain or discomfort. Since it doesn’t break your fast, you can take it as needed without worrying about disrupting your fasting routine.

Managing Pain Without Breaking Your Fast
If you’re concerned about taking Tylenol during fasting, consider these alternatives:
Stay hydrated: Dehydration can exacerbate headaches and muscle pain.
Use MCT oil: While it contains calories, small amounts of MCT oil can provide energy without spiking insulin levels.
Practice relaxation techniques: Stress and tension can contribute to pain, so try deep breathing or meditation.
Unlock the secrets via Amazon
Unlock the secret to effortless fat loss, boundless energy, and radiant health with Intermittent Fasting for Women! This powerful book is your ultimate guide to harnessing the science-backed benefits of fasting, optimized for the female body. Discover how to boost metabolism, balance hormones, and achieve lasting weight loss without restrictive dieting. Packed with expert insights and practical strategies, it empowers you to take control of your health on your terms. This book is your game-changer if you’re ready to transform your body, mind, and confidence. Grab your copy today and step into the healthiest, strongest version of YOU!
Special Considerations for Medical Conditions
Diabetes and Blood Sugar Levels
If you’re taking diabetes medication, monitoring your blood sugar levels closely during fasting is essential. Also, vitamin supplements like vitamin C or vitamin D may interact with your fasting routine, so always consult your health care provider. While Tylenol doesn’t affect blood sugar, combining it with other medications or supplements could have unintended effects. Always consult your healthcare provider before making changes to your medication regimen.
High Blood Pressure and Thyroid Medications
Certain medications, like those for high blood pressure or thyroid conditions, may require food for optimal absorption. If you’re taking such medications, discuss your fasting routine with your healthcare provider to ensure you’re not compromising your health.
Potential Side Effects of Tylenol During Fasting
While Tylenol is generally safe, taking it on an empty stomach can occasionally cause mild stomach upset. Additionally, large doses or prolonged use can lead to liver damage. To minimize risks:
- Stick to the recommended dosage.
- Avoid alcohol, which can exacerbate liver damage.
- Consider pairing Tylenol with a healthy fat (like avocado) during your eating window if stomach upset occurs.
Conclusion
In most cases, Tylenol is safe to take during intermittent fasting. However, if you’re taking other such drugs or supplements, ensure they align with your fasting practice to avoid unintended side effects. It doesn’t contain calories, won’t spike insulin levels, and won’t interfere with the health benefits of fasting. However, it’s always a good idea to consult your healthcare provider, especially if you have a medical condition or are taking other medications.
Remember, intermittent fasting is a tool to enhance your health, not a rigid rule that should cause unnecessary stress. If you need pain relief, don’t hesitate to take Tylenol. Your well-being is what matters most.
By understanding how Tylenol interacts with your fasting routine, you can make informed decisions that support both your health and fasting goals. Whether you’re fasting for weight loss, improved insulin sensitivity, or overall well-being, Tylenol can provide a safe and effective option for pain relief.