Why This Conversation Matters More Than Ever
Intermittent fasting has gone from a niche wellness trend to a widely adopted lifestyle change in recent years, touted for its health benefits like weight loss, better insulin sensitivity, and improved heart health. But what if you’re one of the millions who rely on blood pressure medication while intermittent fasting? Can you safely fast while managing high blood pressure?

That’s exactly what we’re breaking down here.
This guide doesn’t just skim the surface, it dives deep into how different types of fasting interact with blood pressure medicine, and how to plan your medication schedule, food intake, and fasting window for overall health without compromising safety.
What Is Intermittent Fasting?
You’ve probably heard someone rave about intermittent fasting, a friend who swears it helped with weight loss, or a relative who says their energy levels improved. But let’s break it down in a way that feels less like a health lecture and more like a conversation over coffee (yes, black coffee is allowed while fasting, more on that soon).
At its core, intermittent fasting is simply choosing to eat during a specific time period and fast the rest of the day. It doesn’t focus on what you eat as much as when you eat. And this small shift, compressing your eating into a fixed number of hours, can have powerful ripple effects on your body.

Recent studies, including discussions at the American Heart Association Conference, have shown that intermittent fasting may improve insulin sensitivity, support a healthy immune system, and reduce the risk factor for several chronic diseases, including cardiovascular disease and metabolic syndrome.
Different Ways to Practice Intermittent Fasting
You don’t have to go without food for days to see the benefits of intermittent fasting. There are different ways to approach it, depending on your lifestyle, health, and medication needs.
1. The 16:8 Method (Time-Restricted Eating)
This is the most beginner friendly. You fast for 16 hours and eat during an 8-hour eating window. For example, you might eat between 12 PM and 8 PM, and fast the rest of the time.
Best for: People taking morning medications who need food.
2. The 5:2 Method
You eat normally for 5 days of the week, and for the other 2 days, you reduce your calorie intake to around 500–600.
Best for: Those easing into fasting without changing daily medication routines drastically.
3. Alternate-Day Fasting
You eat every other day and fast or consume very few calories on the off days.
This approach can be hard to maintain long-term and may pose a higher risk for people on multiple medications.
4. 24-Hour Fasting
You fast for a full 24-hour period, maybe once or twice a week.
Best attempted under medical guidance, especially if you’re taking medications that affect blood sugar or blood pressure.
Understanding High Blood Pressure and the Role of Medication
What Is High Blood Pressure, Really?
High blood pressure, or hypertension, occurs when the force of blood pushing against your blood vessels is consistently too high, usually above 130/80 mm Hg. Left untreated, it can damage the cardiovascular system, increasing the risk of heart disease, stroke, kidney failure, and heart attack.
Why Medications Matter
Managing high blood pressure isn’t about just popping a pill and calling it a day. It’s a daily commitment, one that affects your heart, energy, mind, and long-term well-being.
Now add fasting to the mix. Suddenly, when you take your meds, what you’ve eaten (or haven’t eaten) becomes critical. That’s why understanding how medications interact with your fasting period is essential.

Here’s a breakdown of common blood pressure medications and what they do:
ACE Inhibitors
These help your blood vessels relax and widen, making it easier for blood to flow and reducing pressure. They’re great for people at higher risk of heart attacks or with other chronic issues like diabetes.
But: they can cause low blood pressure if taken without enough fluids or food, especially during long fasts.
Beta-Blockers
These slow down your heart rate and reduce the force of your heartbeat, lowering your blood pressure. But combined with fasting, they can lead to dizziness or fatigue if your energy levels are already low.
Diuretics (Water Pills)
They help your body get rid of excess sodium and water, reducing blood volume. But fasting often leads to natural fluid loss. Combined with diuretics (like mineral water or low-sodium broth), this can cause electrolyte imbalance, dehydration, and cramping.
Calcium Channel Blockers
These prevent calcium from entering heart and artery cells, which helps your blood vessels relax. But they sometimes need to be taken with food, and taking them during a fasting window may cause stomach upset or reduce absorption.
If your medication regimen doesn’t match your eating pattern, you could face unwanted side effects, from mild dizziness to serious health complications.
How Intermittent Fasting Affects Blood Pressure
Several studies, including a 2019 publication in the journal Cell Metabolism, show that intermittent fasting may lower blood pressure, reduce body weight, and improve cholesterol levels. This is due in part to reduced calorie intake, improved insulin response, and decreased inflammation.

One thing to consider: If you’re already on BP medication, these benefits may come with potential risks if not properly managed.
Comparing Blood Pressure Medication and Intermittent Fasting Impacts
| Aspect | Impact of Fasting | Medication Consideration |
|---|---|---|
| Blood Pressure | Can lower blood pressure over time | Risk of low blood pressure (hypotension) |
| Blood Sugar Levels | Improves insulin sensitivity, may lower blood glucose | Risk of low blood sugar, especially with diabetes meds |
| Electrolyte Balance | May lead to electrolyte imbalance, especially during long periods of fasting | Diuretics may worsen this |
| Heart Rate | May initially drop with caloric restriction | Beta-blockers affect heart rate, needs close monitoring |
| Body Weight | Promotes weight loss, reduces fat stores | Enhances medication efficacy, but adjust under medical advice |
| Timing Conflicts | Fasting window may clash with medication timing | Adjust medication regimen accordingly |
Can You Take Blood Pressure Medicine While Fasting?
Yes, But Only If Done Right
You can take bp medicines while fasting, but it needs proper supervision, especially during alternate-day fasting or 24-hour periods.
Here’s why timing is critical:
- ACE inhibitors taken without food may cause sudden low blood pressure
- Diuretics can worsen dehydration and increase electrolyte loss.
- Beta-blockers combined with low calorie intake may result in fatigue or dizziness.
- Taking medications at the wrong time of day can reduce their effectiveness
Best Way to Combine Fasting and Blood Pressure Medication Safely
1. Consult Your Healthcare Provider
Always start here. Whether you’re trying time-restricted eating or alternate days, your doctor will help you:

- Adjust your medication schedule.
- Monitor diastolic blood pressure and heart rate.
- Ensure no interaction with fat-soluble vitamins, thyroid medications, or iron supplements.
In hypertensive patients, intermittent fasting can be beneficial, but it requires careful adjustments in medication and close monitoring.
2. Align Your Medication Timing With Your Eating Window
Let’s say your meds need food, then you’ll need to schedule your eating window accordingly. If you’re doing 16:8 fasting, consider starting your meals earlier to align with your morning pills. If your fasting period is from 8 PM to 12 PM the next day, you might need to shift your medication timing to early in your eating window to avoid taking it on an empty stomach.
Use pill reminders and talk to your doctor about extended-release versions of your meds.
3. Choose the Right Type of Fasting Plan
Not all fasting is equal. Here are different intermittent fasting schedules you can consider:
- Time-restricted eating (16:8) – Easiest to manage medications
- Alternate-day fasting – May require closer monitoring.
- 5:2 method – Safer for those on prescription medications
- Fasting during daylight hours (like in the holy month of Ramadan) – Requires medication re-timing
Avoid long periods without food if you’re prone to low blood sugar or electrolyte imbalance.
4. Keep Hydration and Electrolytes in Check
During fasting, your body naturally excretes more water. If you’re also on diuretics, the risk of electrolyte imbalance shoots up. Drink plenty of water and consider including mineral-rich broths or electrolyte tablets during longer fasts.

5. Adjust Based on Your Body, Not Just the Clock
Some people need their meds in the morning, others at night. Your fasting schedule shouldn’t be set in stone; it should be adaptable to how your body and your medications interact. Remember, fasting is a lifestyle change, not a punishment.
6. Track Your Numbers
Keep tabs on your blood pressure readings, your heart rate, and how you feel during the day. This helps you and your doctor decide if your fasting plan is helping or hurting.
Common Intermittent Fasting Side Effects While on Medication
You are following the intermittent fasting in the right path, but it’s normal to feel some shifts when you first start fasting; moreover, if you’re on medication, the effects can feel amplified.
Here’s what to expect and how to manage it:
1. Lightheadedness or Dizziness
This often happens when your blood sugar levels drop or if you’ve taken meds without food. It’s more likely if you’re on beta-blockers or ACE inhibitors.
What to do: Adjust your meal timing, especially around your medication timing, and monitor your symptoms.
2. Fatigue or Low Energy
Fasting can dip your energy levels initially, especially if your body is adapting to burning fat instead of glucose. Certain meds can intensify this.
What to do: Add healthy fat sources like avocado or nuts to your meals and avoid over-restricting your calorie intake.
3. Headaches or Muscle Cramps
Often caused by electrolyte imbalance, especially when combining fasting with diuretics.
What to do: Increase your water intake and consider mineral supplements if approved by your doctor.
4. Constipation or Digestive Issues
Reduced food intake and salt intake can slow digestion.
What to do: Stay hydrated and include fiber-rich foods during your eating window.
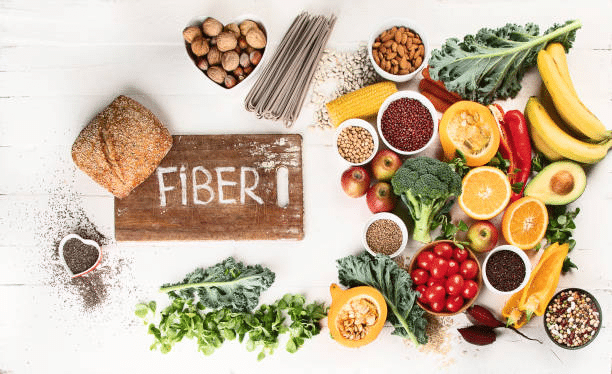
What to Eat During Eating Window – Foods That Support BP & Fasting
Best Foods to Include
- Leafy greens, bananas, and sweet potatoes help lower blood pressure naturally and reduce blood glucose spikes.
- Fatty fish (like salmon), rich in omega-3s, support heart health.
- Healthy fats: olive oil, avocado (key in Mediterranean diet)
- Avocados, olive oil, and chia seeds are high in healthy fat.
- Berries, apples, and whole grains support insulin resistance and stabilize energy levels.
- Nuts and legumes are rich in magnesium and protein.
Foods to Avoid
- Highly processed snacks mess with blood sugar and salt intake.
- Fatty foods that counteract blood pressure medications
- Unhealthy foods rich in sodium and sugar
- Sugary drinks — spike glucose, then crash energy.
- Too much caffeine, even black coffee, can dehydrate if overdone.
- Keto snacks full of artificial ingredients — if following a ketogenic diet, keep it clean and natural.
- Over-the-counter medications without discussing with your doctor

Your eating window isn’t just a green light to eat anything. The right food choices can actually enhance the benefits of intermittent fasting and support your cardiovascular system.
When Intermittent Fasting Might Not Be a Good Idea
While fasting offers many benefits, it’s not for everyone, especially if you’re on medications.
You should pause or rethink fasting if:
- You’re taking multiple counter medications or have complex medical conditions.
- You’ve experienced low blood pressure episodes before
- You’re managing diabetes medications alongside BP meds.
- You have a history of an eating disorder.
- You’re recovering from a serious condition or a heart attack.
- You have advanced cardiovascular disease and require frequent meals.
- You struggle with electrolyte imbalances or dehydration
In these cases, fasting could do more harm than good. That doesn’t mean you can’t make lifestyle changes for your health, but fasting might not be your best tool.
The best guide for every woman on Amazon Kindle
Looking for a breakthrough? This Amazon bestseller isn’t just another self-help guide; it’s a powerful, heartfelt journey packed with real-life wisdom and practical steps to help you grow, transform, and reach your full potential. Written with genuine care by Patricia Nestor, it speaks to your struggles, offering not just advice but a fresh perspective and the motivation to take action.
Change isn’t some distant dream; it’s right here, waiting for you. Don’t wait for the “perfect” moment. The future you want starts with a single step. Open the book, turn the page, and begin your journey today!
Can intermittent fasting lower blood pressure naturally?
Yes. Studies have shown it improves insulin sensitivity, reduces body weight, hypertension, and lowers BP and mm Hg in systolic and diastolic blood pressure.
Does medication break a fast?
Most BP medications do not break a fast unless they are in a syrup, chewable form, or contain calories. But always consult a healthcare provider.
What time of day should I take my medication if I fast?
Ideally, during your eating window. If fasting for a 24-hour period, discuss alternate scheduling or medication types with your doctor.
What are the signs that fasting is affecting my medication?
Feeling faint when standing up, or skipped heartbeats
Fatigue
Cramping
Heart palpitations
These may indicate low blood pressure or electrolyte imbalance.
Is it safe to fast every day while on blood pressure medicine?
Time-restricted eating is generally safe with proper monitoring. Alternate-day fasting or extended fasts should be approached cautiously. One of the safest fasting methods is 16:8.
Do I need to stop fasting if I feel unwell on blood pressure medication?
You may need to pause fasting temporarily. Talk to your healthcare provider immediately; your body might be reacting to low blood pressure, dehydration, or electrolyte shifts.
A Balanced Approach Always Wins
The best way to combine intermittent fasting and blood pressure medication is to stay informed, go slow, and work closely with your doctor. With the right medication regimen, type of fasting, and nutrient-rich food intake, you can enjoy the health benefits of fasting while supporting your cardiovascular system.

With the right approach of an intermittent fasting plan, it can be a powerful tool, not just for managing blood pressure, but for improving your overall health in the long term.
Start where you are. Adjust what you can. And trust that progress, not perfection, creates long-term change.
When you listen to your body and align it with smart choices, you don’t just survive, you thrive.
Let this be the day you move from confusion to clarity. The best results come from honest decisions, personalized routines, and a little patience.



